
American men used to have higher rates of lung cancer, but a new study shows more women are being diagnosed with the deadly disease.
The number of patients being diagnosed with lung cancer has shifted, with higher incidence among younger women now than younger men, according to the American Cancer Society. A new study shows that the trend is also spilling into older age groups of women.
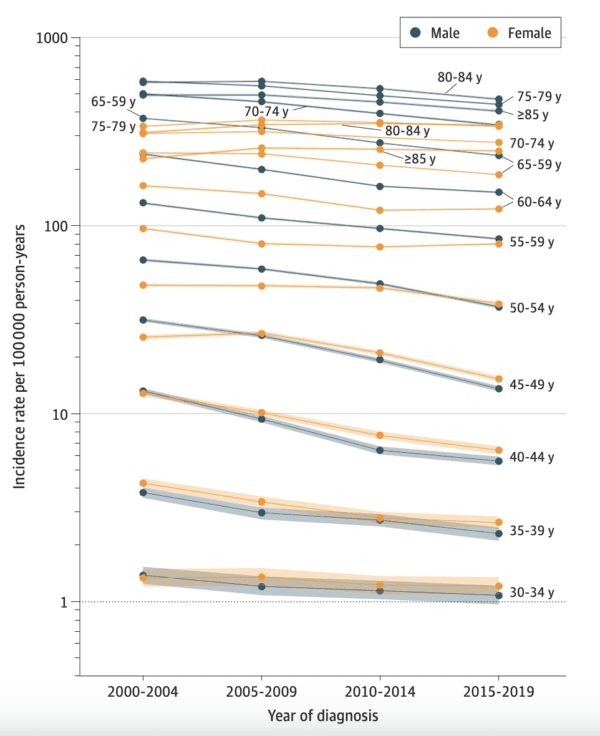
The authors of the paper published in the Journal of the American Medical Association Oncology examined the incidence rates of lung and bronchus cancer diagnoses from 2000 to 2019 in five-year increments, focusing on patient sex, age, and year of diagnosis.
Results of the cross-sectional analysis show a steeper decline in men’s lung cancer rates between 2000 and 2004 and between 2015 and 2019. In contrast, incidence rates in women aged 35 to 54 climbed during these same periods, demonstrating what researchers call a “reversal in the historically higher burden in men.”
In patients aged 50 to 54, the rate per 100,000 people decreased by more than double in men compared with women, showing drops of 44 percent and 20 percent, respectively. This translates to a female-to-male rate ratio increase from 0.73 in 2001–04 to 1.05 in 2015–19. The only women with incidence rates lower than men were those 55 and older. However, the gap narrowed as time progressed.
The study built upon a 2018 paper funded by the American Cancer Society.
A Concerning Trend
The findings are worrisome to researchers not only because of the rising number of women affected but also because not all lung and bronchus cancers stem from cigarette smoking. Many origins of the disease remain unknown.
“We don’t know why lung cancer incidence rates among younger and middle-aged individuals are now higher in women than men, reversing the historical pattern,” Dr. Ahmedin Jemal, senior vice president of surveillance and health equity science at the American Cancer Society and lead author of the paper, said in a statement. “Cigarette smoking prevalence, the major risk factor for lung cancer in the United States, is not higher in younger women than younger men.”
However, earlier science does suggest that women are at a higher risk of developing lung cancer from cigarette smoking. A study published in the American Journal of Epidemiology in 1993 concluded that women had three times the odds ratio of men (27.9 to 9.60) for developing lung cancer because of smoking. A larger study published in the British Journal of Cancer in 2014 concluded that “heavy smoking might confer to women a higher risk of lung cancer as compared with men.”
Asian Women Inherently at Risk?
Asian women may be particularly at risk of lung cancer because of a genetic predisposition—even if they’ve never picked up a cigarette.
In a paper published in Nature Genetics, researchers presented their discovery of three inherited genetic regions that predispose Asian women who have never smoked to lung cancer that are different from those involved in lung cancer linked to smoking.
The comprehensive study spanned 14 studies and included more than 10,000 Asian women who never smoked and controls. The results indicated that variations in the subjects’ DNA at three locations—two on chromosome 6 and one on chromosome 10—were associated with lung cancer in Asian female never-smokers.
Smoking Statistics
According to the U.S. Centers for Disease Control and Prevention (CDC), cigarette smoking remains the leading cause of preventable disease and death in the United States. Up to 90 percent of all lung cancer deaths—which hover close to half a million per year—are linked to smoking. Cigarette smoking costs the health care system about $600 billion annually. As of 2021, nearly 11 percent of Americans smoke.
Dr. Jemal echoed the CDC’s worrisome statistics in the same statement, pushing for greater efforts toward a solution.
“Lung cancer is still the leading cause of cancer death in the U.S., with 80 percent of cases and deaths caused by cigarette smoking,” he said.
To lessen the disease burden among younger and middle-aged women, Dr. Jemal said more resources are needed to promote the cessation of smoking and other tobacco use via community public health efforts and primary health care providers and expand Medicaid benefits to cover the high costs of prevention resources and lung screenings.
“Also, further research is needed to shed light on the reasons for the higher lung cancer incidence in younger and middle-aged women,” he said.
Ways to Help You Quit
It can take eight to 11 attempts to quit smoking, according to a study published in BMJ Open, but it’s possible. The CDC recommends the following strategies to set yourself up for success:
1. Create a Nonsmoking Environment
- Toss all the cigarettes in your home, car, and workplace before you quit.
- Dispose of things you use while smoking, such as lighters, matches, and ashtrays.
- Wash your clothes and anything else that smells of tobacco smoke.
2. Tell People You’re Trying to Quit
- Tell the people you spend time with that you plan to quit. Ask them to support your decision, especially colleagues who currently smoke, by asking them not to smoke around you and to refrain from offering you cigarettes.
- Make it known to your health care team, including primary care physicians, dentists, counselors, pharmacists, and nurses. They can provide extra support and make suggestions on how to quit.
3. Be Mindful of Temptations
- Stay away from places that sell cigarettes.
- Avoid situations in which you’ll be tempted to smoke and cigarettes are available.
- Unsubscribe from any tobacco marketing companies that send you email promotions or pamphlets promoting their products.

