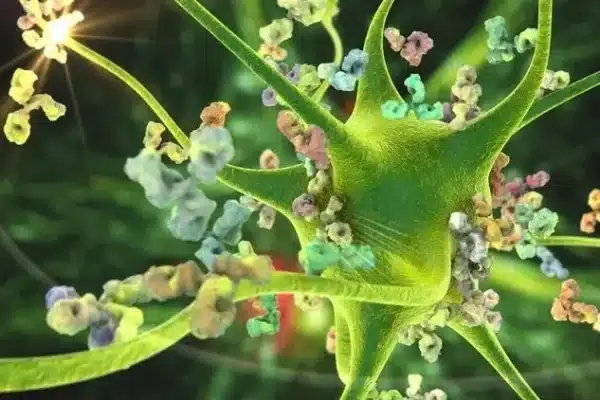
An excessive cytokine storm can lead to prolonged autoimmune responses and trigger specific underlying pathophysiology for disease.
Since the onset of COVID-19, researchers have established a strong association between the SARS-CoV-2 virus infection and cardiovascular and respiratory diseases. Recent research has also revealed a significant increase in the risk of autoimmune and inflammatory diseases due to COVID-19.
The study collected data between Oct. 8, 2020, and Dec. 31, 2021, from the Korea Disease Control and Prevention Agency COVID-19 National Health Insurance Service. This data included 354,527 individuals who were infected with the COVID-19 virus and 6,134,940 individuals who were not infected (the control group). The average age of both groups was approximately 52 years, and the mean follow-up times were 119.7 days for the group infected with the COVID-19 virus and 121.4 days for the control group.
The results revealed that, compared to the control group, the increased risks of developing immune system diseases in the COVID-19 group were as follows: alopecia areata (spot baldness) 1.12 times, alopecia totalis (complete baldness) 1.74 times, Crohn’s disease 1.68 times, sarcoidosis (tiny collections of inflammatory cell growth)1.59 times, and antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis 2.76 times.
The researchers believe that an excessive cytokine storm (an aggressive response by the immune system to infection) leads to prolonged autoimmune responses, consequently triggering the specific underlying pathophysiology for each disease.
Subgroup analysis also revealed that age and gender are associated with the risk of various diseases within the COVID-19 group. Individuals aged 40 and above have a higher risk of developing alopecia areata, alopecia totalis, and ANCA-associated vasculitis, whereas those aged 40 and below have a higher risk of developing Crohn’s disease, sarcoidosis, adult-onset Still’s disease, and rheumatoid arthritis. Additionally, men are more prone to develop alopecia totalis, Crohn’s disease, psoriasis, systemic sclerosis, adult-onset Still’s disease, and ankylosing spondylitis, while women are more susceptible to alopecia areata and alopecia totalis, ANCA-associated vasculitis, sarcoidosis, Crohn’s disease, and vitiligo.
The more severe the COVID-19 virus infection, the higher the risk of developing rheumatoid arthritis, vasculitis, ulcerative colitis, vitiligo, psoriasis, alopecia totalis, Crohn’s disease, adult-onset Still’s disease, Sjögren’s syndrome, ankylosing spondylitis, and sarcoidosis.
The paper’s authors stated, “Autoimmune and autoinflammatory connective tissue disorders may manifest as post-COVID-19 sequelae,” suggesting that long-term management of COVID-19 patients should include evaluation of subsequent development of these disorders.
Exercise can impact all immune cells in both the innate and adaptive immune systems, particularly by enhancing the activity of natural killer (NK) cells, neutrophils, and macrophages after moderate exercise. With long-term regular exercise, the effect on the immune system it induces may act as a natural vaccine against viral infections like COVID-19. This is crucial for high-risk groups, including overweight or obese individuals, and those with insulin resistance or diabetes.
The author recommends moderate-intensity exercise, including strength training, balance and control exercises, stretching, or a combination of activities like walking, weightlifting, lunges, and stair climbing. Indoor exercises such as sitting and standing, squats, sit-ups, and yoga are also beneficial. It is advisable to aim for 150 to 200 or 400 minutes of aerobic exercise per week.
In terms of nutrition, consuming a diet rich in vitamins and minerals can boost immunity, especially for individuals with deficiencies in these micronutrients.
Fruits, vegetables, olive oil, oily fish, nuts, and legumes are all considered functional foods. They contain natural health-promoting components, including polyphenols, terpenes, alkaloids, flavonoids, sterols, pigments, and unsaturated fatty acids. These substances provide immune protection through their antioxidant and anti-inflammatory properties.
Additionally, herbs rich in polyphenols, especially fermented teas (green tea, black tea), yerba maté, and coffee, have been shown to exhibit various benefits on metabolic and microvascular activities, cholesterol and fasting blood sugar lowering, anti-inflammation and antioxidation in high-risk individuals.
Bioactive peptides found in food proteins may elicit various physiological responses associated with immunological, antimicrobial, gastrointestinal, cardiovascular, neurological, and other hormonal activities. These benefits of functional foods contribute to safeguarding the body against COVID-19 and other viral infections.